- +1 832 241 0130
- solutions@aidastech.com
- Houston | Bengaluru | Coimbatore
Ready to level up your RCM process?
Contact us for a free assessment and trial
All that you need to optimize your revenue cycle is right here
Our AIDAS revenue cycle management analytics framework is a powerful platform designed to extract insights from electronic medical records (EMR) systems and enhance RCM. Whether you’re a provider network or an RCM service company, our plug-in solution can seamlessly integrate with your current system, generating performance metrics and key performance indicators (KPIs) that provide valuable insights to inform your decision-making.
Our all-in-one revenue cycle analytics platform delivers a consolidated view of process performances, providing RCM teams with a single version of the truth. Our user-friendly, drag-and-drop feature allows business users to build their dashboards, reports & share them securely with the team.
The “Data Utility” functionality allows for the ingestion, processing, and secure storage of data sourced from EMRs.
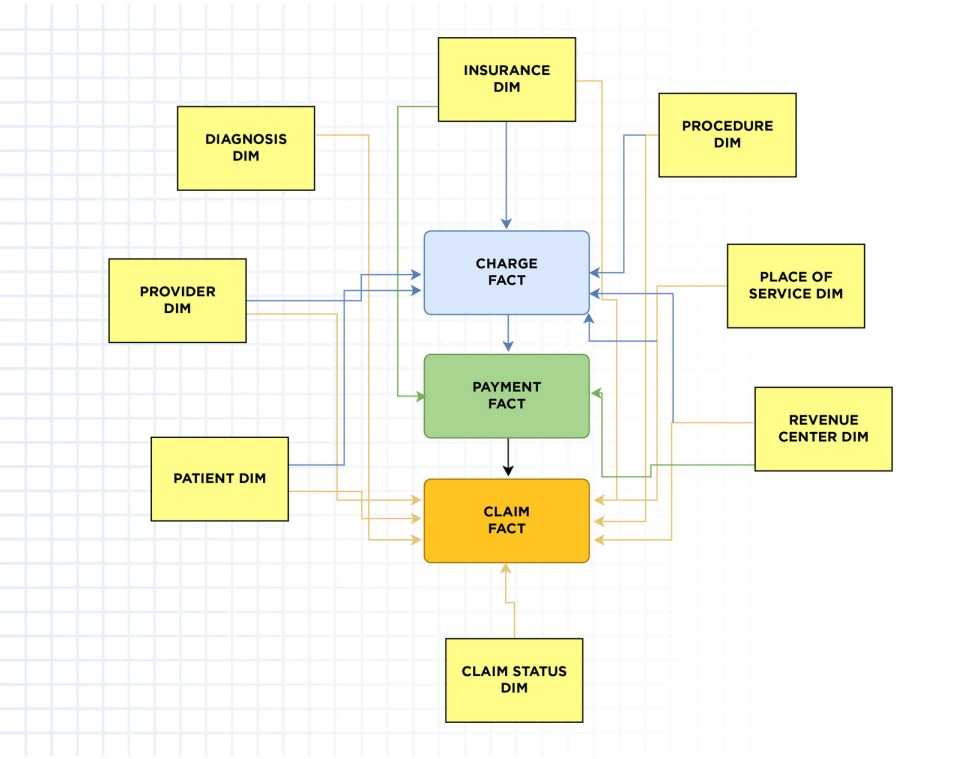
To overcome data silos and enable seamless scalability, we leverage pre-defined data models and pipelines that ensure a standardized data structure. We have built our platform on a robust deployment architecture that incorporates configuration management principles and templates, enabling swift implementation for businesses of any size, regardless of the EMR systems they utilize. This approach ensures a streamlined and efficient setup, allowing you to focus on deriving valuable insights from your data without the complexities of data integration and system compatibility.
The solution has a pre-defined standard data model that stores clean and transformed data for immediate consumption.
The adaptable nature of the model enables customization for individual businesses to add specific data elements. The Data Pipeline feature transforms data from EMR systems into the standard data model while monitoring for data quality and anomalies, supporting standard formats.
Our experts continuously work with IT and data teams to configure and improve the solution over time.
The “Reporting tools” suite offers a comprehensive solution to evaluate the performance of RCM operations, ultimately increasing net revenue. These insights are presented through tailored dashboards and reports, catering to different audiences ranging from executives to analysts, depending on their specific requirements.
Pre-designed dashboards offer a range of KPIs and RCM metrics readily available to start measuring RCM performance.
Operational Reports provide detailed information about claims that require attention across the workflow. Based on business logic, exception reports assist operations teams in planning their day-to-day activities. The reports are available for download in standard formats such as pdf and csv and can be shared with other team members.
“Build Your Own” is a scalable feature that empowers users to analyze and create custom reports based on appointments, charges, payment data and other parameters.
The “Reporting tools” suite offers a comprehensive solution to evaluate the performance of RCM operations, ultimately increasing net revenue. These insights are presented through tailored dashboards and reports, catering to different audiences ranging from executives to analysts, depending on their specific requirements.
Pre-designed dashboards offer a range of KPIs and metrics readily available to start measuring RCM performance.
Operational Reports provide detailed information about claims that require attention across the workflow. Based on business logic, exception reports assist operations teams in planning their day-to-day activities. The reports are available for download in standard formats such as pdf and csv and can be shared with other team members.
“Build Your Own” is a scalable feature that empowers users to analyze and create custom reports based on appointments, charges, payment data and other parameters.
We have already covered some use cases, such as:
The No Surprises Act: Automating good faith and other cost estimates can be time-consuming and require significant manual effort. The pre-defined workflow in our platform automates these estimates and generates reports that benefit providers and patients alike. This improves customer satisfaction, billing and accuracy, and ultimately, revenue.
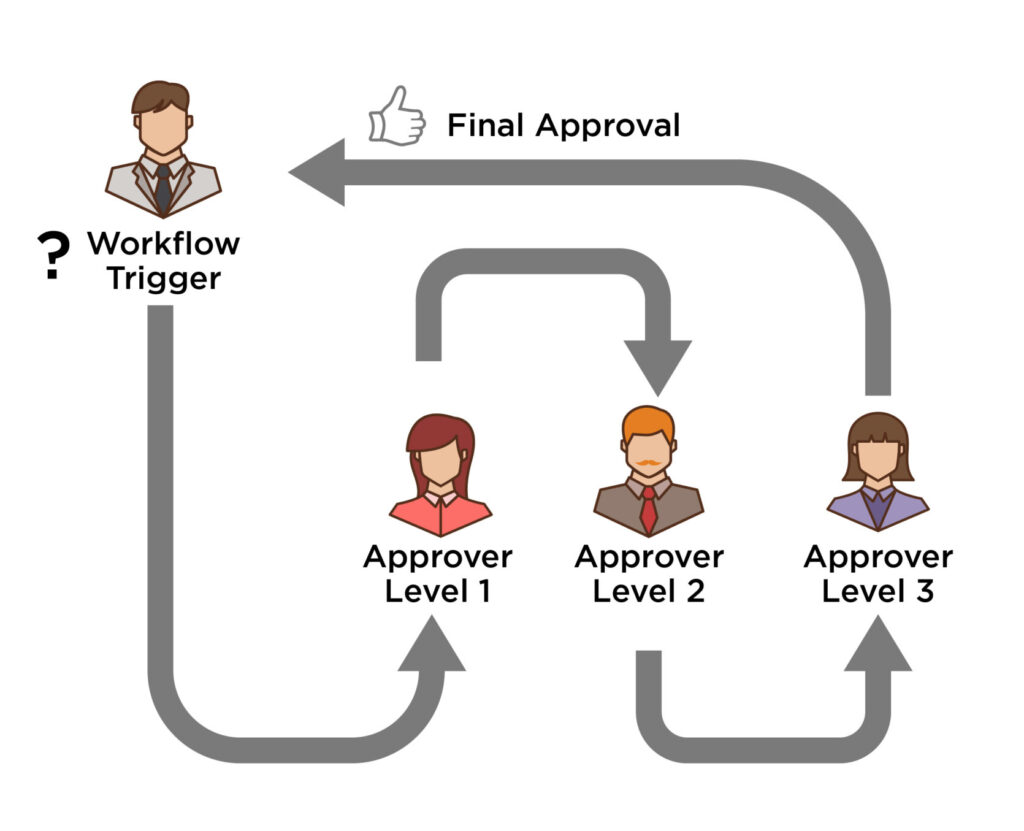
Automated Claims Submission (CS): Our pre-defined CS workflow helps submit timely error-free claims, reducing overall costs. Not only does this automation result in a 2X increase in productivity, it also reduces processing delays and rejections. Highly customizable and easy to build, workflows can be defined and scheduled to run automatically, improving the overall productivity of RCM processes.
If you require more in-depth analysis beyond the scope of dashboards and reports, our analysts can assist you with advanced analytics using statistical methods. Our analysts are experts in deploying appropriate techniques, such as causation, in understanding the relationship between cause and effect.
Drivers of charges per claim: We analyze the distribution of charges per claim and test them against clinical mix and practice differences to determine what drives the pattern.
Underpayment analysis: Our correlation analysis helps to identify variables that lead to higher payments-to-claim ratios, aiding in managing write-offs and recovering significant amounts of revenue.
Contract adherence: Analyzing the reimbursement of the top 10 commercial payors for the top 25 current procedural terminologies (CPTs) compared to Medicare’s current rates can help improve full reimbursements.
Our team of expert analysts is available to understand your business processes and connect them with data to uncover hidden insights that answer unanswered questions.
If you require more in-depth analysis beyond the scope of dashboards and reports, our analysts can assist you with advanced analytics using statistical methods. Our analysts are experts in deploying appropriate techniques, such as causation, in understanding the relationship between cause and effect.
Drivers of charges per claim: We analyze the distribution of charges per claim and test them against clinical mix and practice differences to determine what drives the pattern.
Underpayment analysis: Our correlation analysis helps to identify variables that lead to higher payments-to-claim ratios, aiding in managing write-offs and recovering significant amounts of revenue.
Contract adherence: Analyzing the reimbursement of the top 10 commercial payors for the top 25 current procedural terminologies (CPTs) compared to Medicare’s current rates can help improve full reimbursements.
Our team of expert analysts is available to understand your business processes and connect them with data to uncover hidden insights that answer unanswered questions.
Our analytics platform offers a range of predictive models built on AI and ML technologies to enable businesses to gain insights into RCM metrics.
The platform includes pre-built models to tackle common RCM challenges.
The Denials Prediction Model combines a machine learning model and a rules engine to predict claim denials before they occur. This enables teams to avoid denials and ensure claim success proactively.
The Days to Pay Payer Model uses a well-trained machine learning model to predict remittance dates for each claim. This helps businesses manage their cash flow and allocate resources effectively to collect payments.
The Propensity to Pay model segments patients based on their likelihood to pay. With additional third-party data, this model can also determine charitable eligibility. By focusing collection efforts on high-likelihood claims, this model can help businesses improve their collections process.
Moreover, our platform features a drag-and-drop interface that allows business users to build and deploy custom machine-learning models to address gaps in their RCM processes.
Contact us for a free assessment and trial
AIDAS is a specialized firm in analytics technology & services, helping clients to solve complex business problems using Artificial Intelligence and Machine Learning. We bring expertise in Data Engineering, Analytics Technology, and Consulting to deliver holistic AI-driven insights and solutions to solve problems. Ready to deploy accelerators, a flexible service model, and in-depth experience in putting AI algorithms and Machine learning to practical use makes us a trusted partner to provide value across the enterprise.
Copyright © 2023 – Aidas Technologies. All Rights Reserved.
You already submitted the form!