Business Challenge
One of our clients, a leading healthcare provider based in the US, faced a significant challenge with medical claim denials. These denials, encompassing eligibility mismatches, coding errors, duplicate claims, and appeals, were causing considerable disruption. Notably, 70% of these denials were preventable, straining their Revenue Cycle Management (RCM) processes and impacting financial health.
Solution
We deployed our Denial Predictor on the client’s historical claims data to address the multifaceted denial issues. This tool, integrating advanced technologies such as Natural Language Processing (NLP) and Machine Learning (ML), is capable of identifying and resolving different denial categories.
The tool comprised different modules, each designed to address specific aspects of denial categories the client encountered. The following are some of the major functions of the modules.
- Ensured accurate insurance coverage, especially for Medicare/Medicaid claims.
- Verified correct coding using a comprehensive database of procedure codes.
- Used smart AI logic to identify and score potential duplicate claims.
- Identified and flagged high denial CPT code – Insurance combinations.
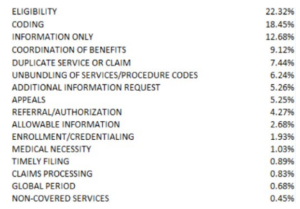
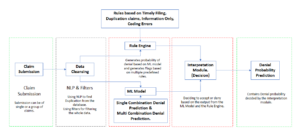
This table represents the different denials the Above is the workflow of our advanced denial predictor tool, the client was facing leveraging the capabilities of machine learning
Impact
The application of the Denial Predictor resulted in a notable 30% reduction in predicted denials. Implementing the Denial Predictor has also led to refining the Revenue Cycle Management (RCM) process. This refinement has translated into faster payment cycles for the healthcare provider. The optimized RCM process ensures that claims are processed more expeditiously, improving operational efficiency and reducing the time it takes to receive payments.